They Were Cigarette Smokers. Then a Stroke Vanquished Their Addiction.
[ad_1]
Taking a scan of an injured brain often produces a map of irretrievable losses, revealing spots where damage causes memory difficulties or tremors.
But in rare cases, those scans can expose just the opposite: plots of brain regions where an injury miraculously relieves someone’s symptoms, offering clues about how doctors might accomplish the same.
A team of researchers has now taken a fresh look at a set of such brain images, drawn from cigarette smokers addicted to nicotine in whom strokes or other injuries spontaneously helped them quit. The results, the scientists said, showed a network of interconnected brain regions that they believe underpins addiction-related disorders affecting potentially tens of millions of Americans.
The study, published in the scientific journal Nature Medicine on Monday, supports an idea that has recently gained traction: that addiction lives not in one brain region or another, but rather in a circuit of regions linked by threadlike nerve fibers.
The results may provide a clearer set of targets for addiction treatments that deliver electrical pulses to the brain, new techniques that have shown promise in helping people quit smoking.
“One of the biggest problems in addiction is that we don’t really know where in the brain the main problem lies that we should target with treatment,” said Dr. Juho Joutsa, one of the study’s lead authors and a neurologist at the University of Turku in Finland. “We are hoping that after this, we have a very good idea of those regions and networks.”
Research over the last two decades has solidified the idea that addiction is a disease of the brain. But many people still believe that addiction is voluntary.
Some independent experts said the latest study was an unusually powerful demonstration of the brain’s role in substance use disorders. Among smokers who had strokes or other brain injuries, those with damage to a particular neural network experienced immediate relief from their cravings.
The researchers replicated their findings in a separate group of patients with brain injuries who completed an alcoholism risk assessment. The brain network associated with a lower risk of alcohol addiction was similar to the one that eased nicotine addiction, suggesting that the circuit may underlie a broader set of dependencies.
“I think this could be one of the most influential publications not only of the year, but of the decade,” said A. Thomas McLellan, professor emeritus of psychiatry at the University of Pennsylvania and a former deputy director of the Office of National Drug Control Policy, who was not involved in the study. “It puts to rest so many of the stereotypes that still pervade the field of addiction: that addiction is bad parenting, addiction is weak personality, addiction is a lack of morality.”
Read More on Smoking and Vaping
In recent years, a succession of studies had identified particular brain regions where a lesion, or injury, appeared to be associated with relief from addiction. But the targets kept shifting.
“People had not been successful in showing consistency in the areas that are involved,” said Dr. Hamed Ekhtiari, an expert in addiction treatments at the Laureate Institute for Brain Research in Tulsa, Okla.
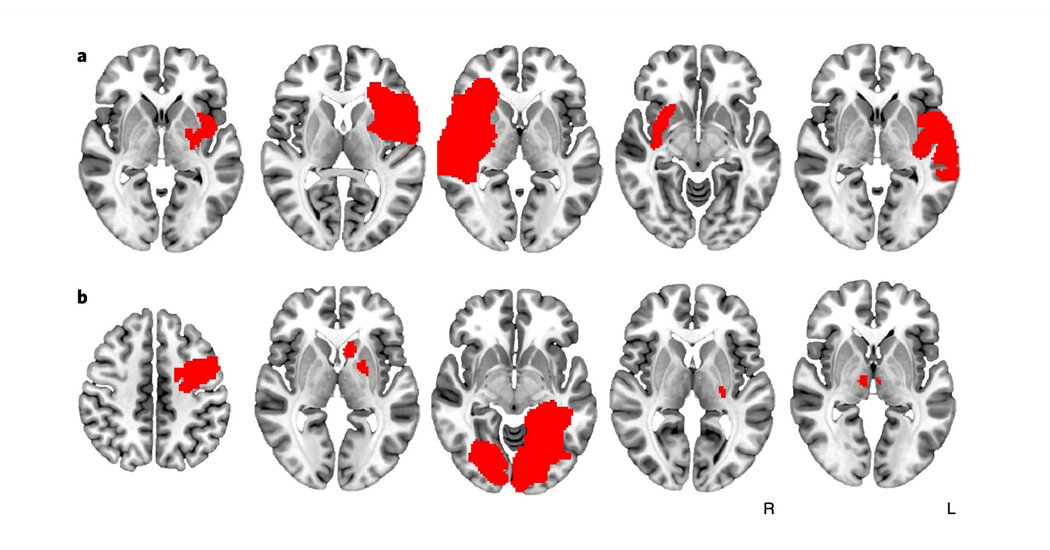
In the new study, Dr. Joutsa applied sophisticated statistical techniques to an old set of brain scans from smokers in Iowa who had suffered neural injuries. An earlier analysis of the same scans had suggested that patients with damage to the insula, a brain region involved in conscious urges, became more likely to quit smoking.
But Dr. Joutsa, going back over the same scans pixel by pixel, noticed that many patients without insula injuries had also lost the urge to smoke. “There was something in the insula story, but it wasn’t the whole story,” he said.
Working with Dr. Michael Fox, an associate professor of neurology at Harvard Medical School, Dr. Joutsa examined a second set of scans from smokers who had suffered strokes in Rochester, N.Y. In all, they looked at 129 cases.
The team struggled to find individual brain regions where injuries reliably helped patients quit smoking. Instead, the researchers turned to standard diagrams of brain connectivity that chart how activity in one region is correlated with activity in another.
Suddenly, the researchers could locate networks of connected brain regions where injuries caused instant relief from nicotine cravings and other networks where injuries did not.
“What we’re realizing across many different fields is that our therapeutic targets are not brain regions, as we once thought, but connected brain circuits,” Dr. Fox said. “If you take into account the way the brain is connected, you can improve treatment.”
The study did not account for how the home lives of patients — how often they were exposed to cigarettes, for example — may have affected their habits. Patients deemed to have gone into addiction remission after their injuries generally quit smoking immediately, reported having no urge to smoke and did not start again while they were being followed.
The researchers did, though, look at whether other changes associated with the injury — to intelligence or mood, for instance — could have helped explain the disappearance of nicotine cravings in some patients. They did not ultimately seem to make a difference.
Outside experts said that parts of the brain network identified in the study were familiar to them from earlier research. Dr. Martijn Figee, a psychiatrist at the Center for Advanced Circuit Therapeutics at Mount Sinai in Manhattan, studies how electrical impulses delivered to the brain can treat obsessive compulsive disorder, depression and addiction. He said that addiction generally seemed to be associated with under-activity of the brain’s cognitive control circuit and over-activity of reward-related circuits.
By applying electrical stimulation on the surface of patients’ heads or using more invasive methods like deep brain stimulation, doctors can suppress activity in certain regions, mimicking the effect of an injury, and excite activity in others. The study identified one region, called the medial frontopolar cortex, that appeared to be a good candidate for excitatory stimulation; that region overlapped with the target of a treatment recently approved by U.S. regulators for helping smokers quit.
That treatment uses an electromagnetic coil placed against a patient’s scalp to deliver electric pulses to the surface of the brain. Other techniques involve implanting electrodes into certain brain regions or permanently deactivating precise brain regions.
“This paper is really interesting in that it clearly indicates some accessible targets” for treatments, Dr. Figee said.
While brain stimulation has become more common for treating depression and obsessive compulsive disorder, the use of those therapies for addiction has been slower to catch on. Researchers said that it would take years to hone the techniques.
Despite studies showing that electrical or magnetic stimulation can reduce craving for addictive substances, it is not clear how long those effects last. Some of the most promising targets are deep in the brain; reaching them can require deep brain stimulation or a specific kind of coil that only became available recently, Dr. Figee said.
Knowing where to direct brain stimulations also does not resolve the question of what frequency to use, scientists said. And the connections are different in different people’s brains, raising the prospect of needing to tailor treatments.
People with addictions have been slower to embrace brain stimulation than have those with depression or movement disorders, researchers said, reflecting in part the taboo around thinking of addiction as a brain disorder.
There may also be structural challenges. Judy Luigjes, an assistant professor of psychiatry at Amsterdam University Medical Centers, recruited from a pool of thousands of patients at addiction treatment centers in the Netherlands for a study of deep brain stimulation. In three years, only two patients started the trial.
Dr. Luigjes and her colleagues wrote that substance use disorder patients may have avoided the procedure in part because their motivation to address the disease fluctuated more than it did in patients with obsessive compulsive disorder.
And the very instability that often accompanies substance use disorders can make investing in time-intensive treatments more difficult. Only one-third of the patients with an appointment with the research team brought a family member or friend, Dr. Luigjes found.
Some scientists are working to address those concerns. An addiction team at Mount Sinai, for instance, has taken to administering less invasive brain stimulation to patients at home or at community centers rather than in the hospital, lowering the barriers to treatment.
But while the brain may be an entry point for treating addiction, Dr. Luigjes said that it was probably not the most important one. Other scientists, too, have argued in recent years that focusing on the brain disease model of addiction has diverted attention and money from research addressing social and environmental factors that contribute to addiction.
“We’ve put too much of our hopes and money and energy into one side,” she said, referring to the field’s focus on brain stimulation. “I don’t know if it will pay out in the way we thought it would.”
[ad_2]